How immersive research revealed that one quiet task—report writing—is breaking the entire behavioral health system.
What Goes Into a Diagnosis? Everything.
The hands-on approach that we took for research let us see the nuance in the assessment-report-diagnosis process. We sat in on intake sessions, watched how clinicians toggled between paper notes and digital records, and studied how long it took to translate a stack of test scores into a coherent, evidence-based report. It was cognitively intensive, emotionally draining, and structurally inefficient.
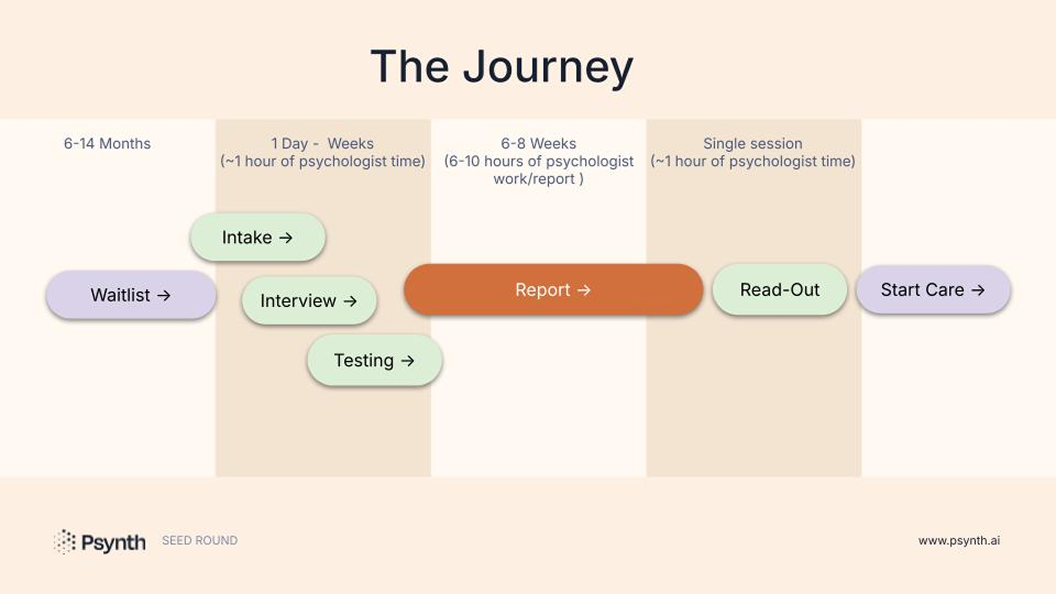
Here’s what the process looks like for a single assessment:
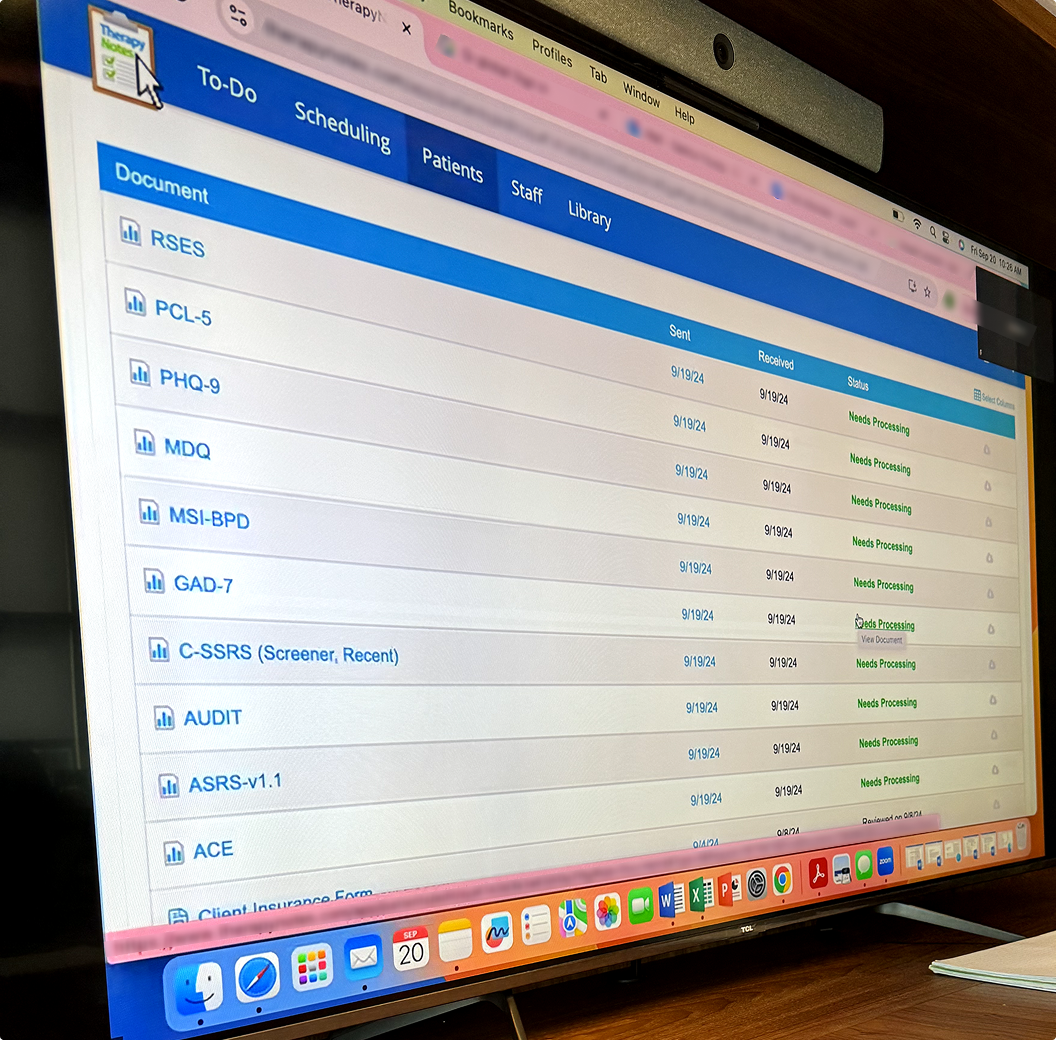
- Patients (or parents) fill out long intake forms.
- Psychologists conduct 1–2 hours of interviews.
- Patients complete 3–12 different cognitive and behavioral assessments.
- The clinician then spends 6–8 hours synthesizing all of this into a formal report: reviewing scores, writing narrative summaries, comparing findings to diagnostic criteria, and rendering a final diagnosis and treatment recommendations.
The work is rigorous—and it should be. But the sheer volume of manual synthesis required has become a bottleneck that slows down access to care at scale.
Validated by the People Who Know the Problem Best
After our field research, we launched a structured interview sprint with 25 psychologists from across the country. The goal was to test the edges of the problem. Was this just one segment’s pain point—or was it industry-wide? What we found was near-universal alignment:
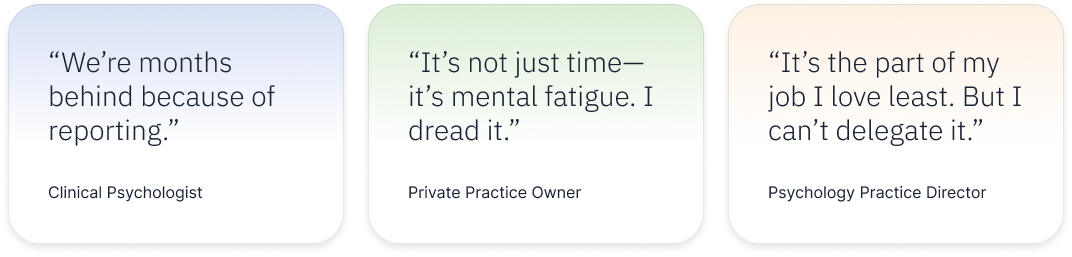
This wasn’t just a task psychologists disliked—it was actively limiting patient throughput, causing clinical burnout, and creating significant operational drag on otherwise thriving practices.
Unbillable Work, Unsustainable Pressure
We dug into the financial model behind assessments. Psychologists can typically bill for the evaluation session and the testing—but report writing is severely under-reimbursed. Psychologists may only get paid for 8 hours of scoring, data entry, and analysis, though a comprehensive report may require over 12 hours.
This means clinicians are doing hours of unpaid work, at night, just to keep up. And hiring help doesn’t solve it—only licensed professionals can sign off on these diagnostic reports.
So they fall further behind. Waitlists grow. Patients suffer.
A Root Cause Hiding in Plain Sight
The deeper we went, the clearer it became: report writing isn’t just a symptom—it’s a root cause.
- It creates patient bottlenecks
- It limits practice scalability
- It drives clinician burnout
- And it drags down the entire diagnostic timeline
While many startups chase innovation in testing or telehealth delivery, few touch the messy, cognitively hard work that happens between input and diagnosis. That’s exactly where we decided to go.
Why This Problem Is Perfect for AI
Unlike tasks requiring physical presence or emotional nuance, report synthesis is exactly the kind of work that’s primed for cognitive automation. It’s rules-based but requires flexible thinking. It follows templates but demands personalization. It’s tedious but mission-critical.
In short: it’s what generative AI was built for.
And it became clear: if we could build a system that synthesized raw clinical data into defensible diagnostic drafts, we wouldn’t just be saving time. We’d be transforming access to care at scale.